When Ben Los’s five-year-old son began suffering from seizures in 2022, Los and his wife sought treatment near their home in Colorado Springs, Colorado, and brought him to a pediatric neurological clinic in Denver to receive an EEG and a diagnosis.
Both Los and his wife are employed as teachers. Los was careful to ask whether their insurance provider covered the procedure. The office assured him that it was covered.
Several months after Los’s son received treatment, Los received two bills totaling more than $2,500, with no explanation of the charges. He was confused and outraged.
Los called the pediatrician’s office and learned that it was actually owned by a large hospital system. The charge was a “facility fee” added by the hospital — essentially a fee for overhead, separate from the services provided. Los spent hours calling the hospital itself but struggled to connect with anyone who could address the problem.
“It was deeply frustrating,” Los, 38, says. “Certainly, there was nothing they mentioned during the initial visit about having to pay the hospital.”
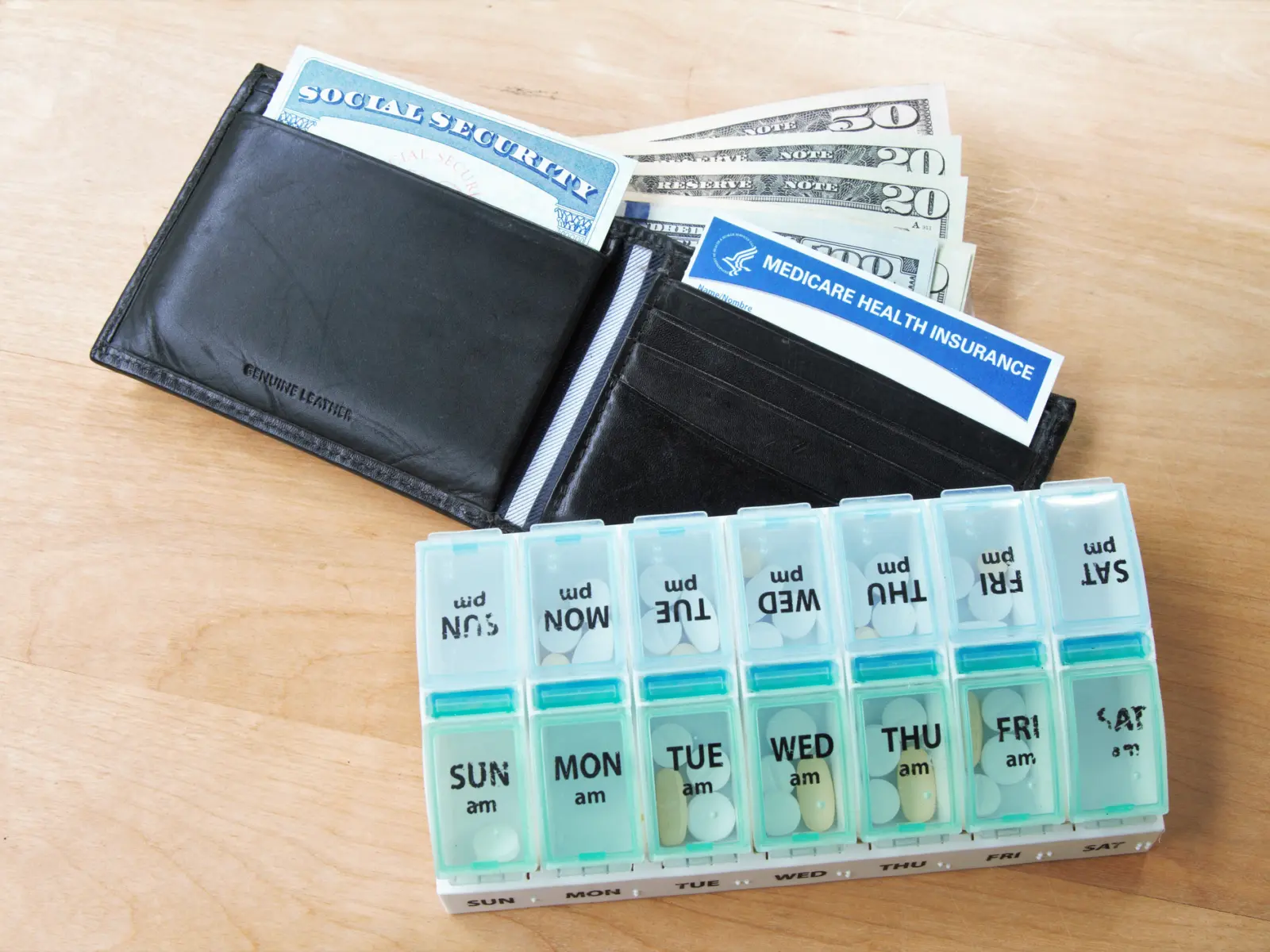
Patients across the country face a similar dilemma. In many states, health care providers have been consolidated under just a few large health systems. Today, a majority of physicians are employed by hospitals and health systems rather than standalone practices. This consolidation reduces competition and drives up prices. And when large hospitals buy up small physician practices, they can also tack on facility fees for services on top of insurance co-pays, making procedures cost two to three times as much for patients as they would at an independent doctor’s office.
These charges are painful for consumers. In Los’s case, the fee put his family under financial stress exactly when they didn’t need it — in the middle of moving.
“Patients are really feeling these facility fees,” says Hunter Kellett, director of health care at Arnold Ventures. “It feels egregious. If you’re getting a routine preventative service that you could get at a regular doctor’s office, there’s just no rationale for charging patients an additional facility fee.”
In Colorado, advocates at the Colorado Consumer Health Initiative (CCHI) encouraged lawmakers to address this problem by passing legislation that checks the practice of charging patients unreasonable facility fees.
“The ability to charge facility fees is one of the incentives that have driven hospitals to acquire more provider practices,” says Isabel Cruz, policy director of the CCHI. “We were trying to tackle their ability to push up costs and increase their revenue by limiting the ability to charge facility fees in office care settings outside of the hospital.”
We were trying to tackle their ability to push up costs and increase their revenue by limiting the ability to charge facility fees in office care settings outside of the hospital.Isabel Cruz policy director for the Colorado Consumer Health Initiative
Despite fierce opposition from the hospital industry, a bill was signed into law that puts several important measures in place. First, it creates a system of patient notification and transparency requirements so that patients receive an estimate of any facility fees up front and aren’t surprised by them at the time of billing. Second, it establishes limitations on the facility fees that can be collected from patients for preventive services. Finally, it creates a task force to further study facility fees, a measure that will help the legislature consider future laws and regulations.
With this step, Colorado joins a growing movement of states across the political spectrum — including Indiana, Texas, Connecticut, New York, and Maine — that are pushing policies to rein in these predatory billing practices by hospital systems.
Bipartisan Agreement on Limiting Facility Fees
Both red and blue states are passing reforms to lower commercial health care prices, indicating a rare but growing bipartisan consensus.
In May, Indiana passed a bipartisan law that prevents large hospital systems from charging patients additional facility fees for services provided at hospital-owned facilities off the hospital’s main campus. The change, which takes effect in 2025, will lower medical bills for people with commercial insurance.
Connecticut has also prohibited certain kinds of facility fees, including fees for telehealth visits, and created transparency measures for medical billing. This year, Connecticut passed a new bipartisan law that expands on those limitations. Beginning in 2024, facility fees will be prohibited for certain services provided on hospital campuses.
Other states are making similar efforts. In 2022, New York passed legislation that prohibits facility fees for all preventative care, a change that took effect in June. This year, Maine passed a law that establishes a task force to further study medical facility fees, building on a 2005 law that prohibits certain fees. Texas also introduced legislation related to facility fees — while the bill did not ultimately pass, its consideration reinforces the growing bipartisan agreement on this issue.
A recent report by Christine Monahan, an assistant research professor and faculty member at the Center on Health Insurance Reforms at Georgetown University’s McCourt School of Public Policy, finds state-level momentum in protecting consumers from unwarranted facility fees in the commercial market. The report shows that states are looking to policies such as prohibitions on facility fees, out-of-pocket cost protections for consumers, consumer disclosure requirements, hospital reporting requirements, and provider transparency requirements.
“It’s a gradual effort because the states that are acting are doing so in the face of significant opposition from the hospital industry,” Monahan says. She added, “It’s inspiring to see.”
Even with positive momentum, much more reform is needed to protect patients from unfair billing and rising health care costs more broadly, and federal policymakers are beginning to feel pressure to address these issues.
Building Toward Federal Action
On Capitol Hill, lawmakers are now debating a set of policies aimed at addressing pricing distortions in both the Medicare program and the commercial sector. Estimates from the Committee for a Responsible Federal Budget say the proposals targeting Medicare alone could save taxpayers more than $150 billion in the next 10 years.
In the House of Representatives, three relevant committees have each marked up related legislation. A bill is now moving through the House that would establish stronger billing transparency in the Medicare system and expand “site-neutral” payments for drug infusion services. (Site-neutral is a term that means patients pay the same amount for medical services no matter where those services are provided.) In general, there is broad bipartisan support in the House on this topic, and the House may vote on this package as early as this month.
Increasing transparency around the billing and the claims would be important in providing more data about the location and scope of predatory billing.Christine Monahan assistant research professor and faculty member at the Center on Health Insurance Reforms at Georgetown University’s McCourt School of Public Policy
“Increasing transparency around the billing and the claims would be important in providing more data about the location and scope of predatory billing,” Monahan says. “If the federal government wants to target reforms, that will give a better sense of what they should focus on and what effect it will have. Right now, one of the struggles is that there’s not a lot of good, reliable information about how bad the problem is and how much benefit reforms will have.”
In the Senate, Sen. Bernie Sanders, chairman of the Health, Education, Labor, and Pensions Committee, recently shared a sweeping bill that prohibits hospitals from charging patients with commercial insurance a facility fee for off-site services, on-site primary care, telehealth, and low-complexity services. It also caps hospital fees at the median amount paid when services are provided in a physician’s office.
Monahan says that Sen. Sanders’s draft bill is the first detailed proposal she has seen from a federal lawmaker that implements site-neutrality in the commercial market.
For his part, Los spent weeks making back-and-forth phone calls with representatives in various offices of the hospital that owns the clinic his son visited, trying to contest the unreasonable facility fees he was charged.
“I don’t remember how many hours I spent on the phone, nor how many different people I talked to, but it was basically an all-consuming endeavor in my off-work hours, leaving insufficient time for parenting on a number of days,” he says.
In the end, he used his own ingenuity to deal with the problem, telling his story to a local TV news station. At that point, hospital representatives became more willing to talk about options. After nearly an hour of debate and haggling, he says, the hospital offered to decrease the facility fee by 75%. He reluctantly accepted, cutting his losses.
That the hospital was ultimately flexible on the amount of the fees, Los says, confirmed his suspicion that it was a “bogus charge” in the first place. He finds that friends across the political spectrum intuitively agree with the injustice of such fees.
“If you’re an ordinary person, I don’t need to explain why a surprise $2,500 bill is so egregious,” Los says. “The only people who are making the opposing argument are trying to stand up for hospitals’ corporate profits.”
Los contributed written testimony about his experience to hearings of the Colorado General Assembly on the bill to limit hospital facility fees, and he was gratified when it passed. He believes future legislation should go farther.
“The best approach is making sure that facility fees are banned outright,” Los says. “People should know, in one single bill, what it is that they’re going to be charged. There should be no obfuscation about what the total charge should be.”