Surprise medical billing was a serious problem for American families long before COVID-19 struck. While the circumstances have changed, the need for surprise billing protections has not. In fact, protections are needed now more than ever for all patients.
As the virus spreads, people will be desperately seeking diagnosis and treatment in any available setting — including the emergency room — and for insured patients, that care may often be out-of-network. President Trump recently announced that providers receiving funding from the $100 billion bailout fund included in the third COVID-19 stimulus package must refrain from surprise billing COVID-19 patients. However, there are a number of questions about how this requirement will be implemented, and even with it, major gaps in patient protections remain.
Patients who have been tested and treated for COVID-19 shouldn’t subsequently be hit with surprise bills. It is important that patients feel they can seek the care they need for COVID-19 without risking their financial security. Keep in mind that some of the people needing testing and treatment are the very same front-line providers — such as nurses — who are caring for patients. We shouldn’t reward their service with unaffordable bills.
To be clear, a small subset of providers actually engage in surprise billing. These bills in the emergency room are often generated by private equity-owned physician groups who charge patients 500 to 800 percent more than Medicare rates for out-of-network services. This was price gouging before the current crisis, and it is price gouging now. At the same time, recent reports have indicated that these same firms are laying off providers or cutting their pay — while simultaneously asking for federal funding from the hospital bailout fund.
Congress needs to enact legislation as part of the emergency response bills or another bill that:
1. Prohibits all providers from directly billing insured patients.
2. Limits what these providers are paid when they present their surprise bill to the insurer.
Demanding excessive prices raises costs for patients, employers, and taxpayers, creating additional affordability challenges and slowing the time for the economy to recover.
Congress has legislation before it now that could solve this problem in a comprehensive manner that is fair to the patients, employers, and taxpayers that pay for care — and to those providing care.
All ideas proposed eliminate surprise bills for patients and require them to pay whatever they would’ve paid for the same care in-network. But lawmakers disagree on how to address payment rates for the out-of-network services, an important consideration with implications for health care spending — pitting the providers who want to continue to extract excessive charges against the consumers, employers, and taxpayers who have to pay them.
To end surprise billing and lower U.S. health care spending, the most effective approach is a payment benchmark requiring insurers to pay providers a local, market-based rate. This approach — which would result in savings to consumers, employers, and taxpayers — is included in several bipartisan bills that have advanced out of House and Senate committees.
Opponents to this approach have asserted a number of myths about surprise billing and this proposed solution. Below, we address and debunk these myths.
Myth 1: Insurance companies — more than any other group — stand to benefit from the windfall in savings that would result from establishing a locally-based market rate for out-of-network care.
Reality: Patients and taxpayers are the main beneficiaries of the savings that arise from fixing surprise billing. The savings arising from a benchmark approach would lead to lower premiums for consumers and employers, higher wages for American families, and savings to the taxpayer.
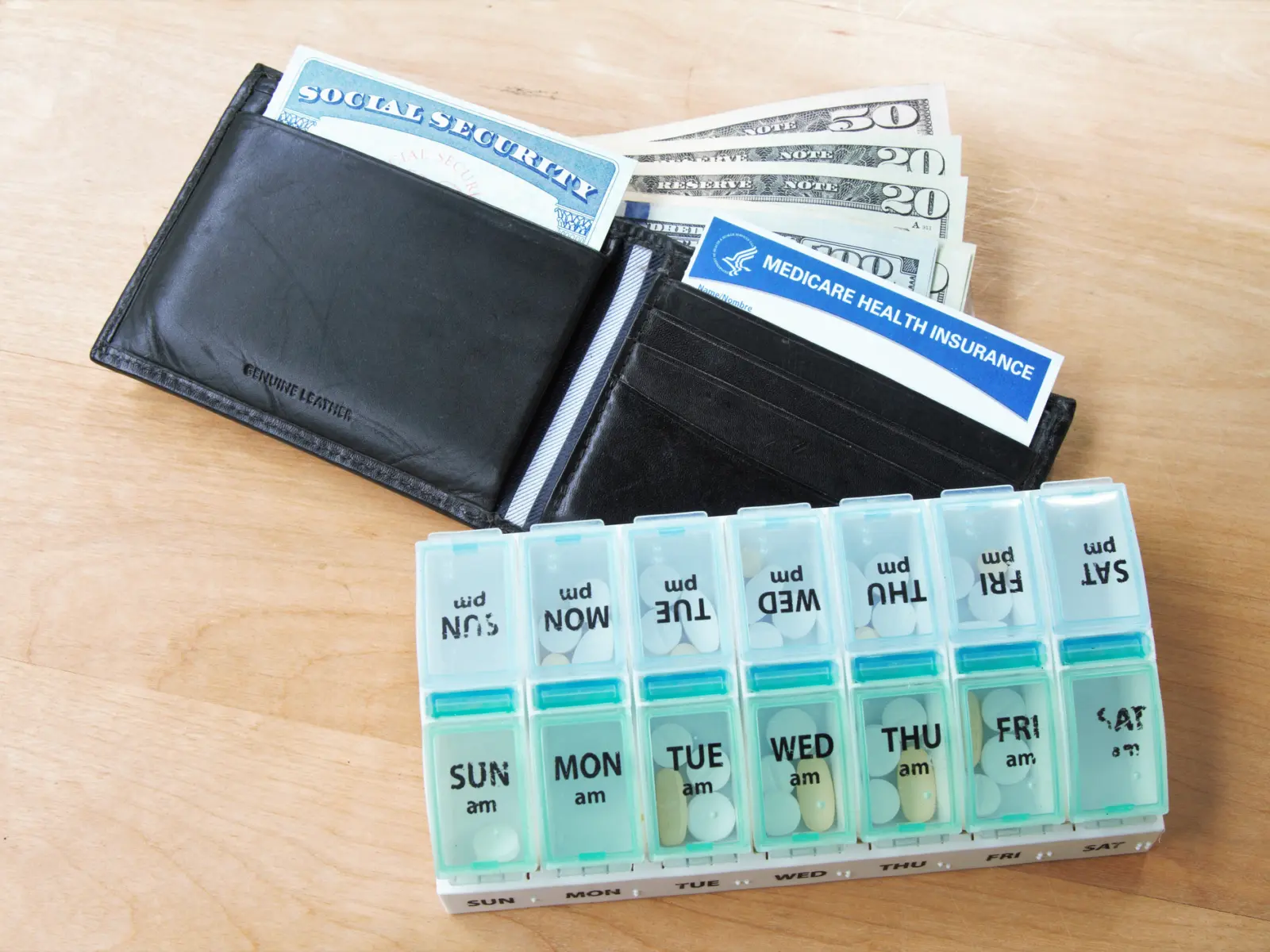
Receiving a surprise bill can be economically devastating for the average American family. In September 2018, one in 10 insured adults said they received a surprise bill in the previous year, and in 2016, more than 40 percent of emergency department visits and inpatient admissions at in-network facilities resulted in a surprise bill. The average surprise bill exceeds $600, which is far more than what 40 percent of families would be able to pay without borrowing or selling something. In addition to the direct impact on those receiving the bills, surprise billing also has a broader impact on consumers — driving up health care costs and premiums and reducing wages.
Surprise billing has inflated premiums by more than 3 percent, roughly a $40 billion increase in health care costs annually, according to research by Zack Cooper and his colleagues. Surprise billing solutions should put downward pressure on inflated rates for out-of-network care, which will not only lower health care premiums for American families, but will also result in an increase in their paychecks. This linkage between health care premiums and wages has been well-established in the economics literature. The Joint Committee on Taxation (JCT) and Congressional Budget Office (CBO) concluded in 2019 that premium savings arising from this change to surprise billing would ultimately flow back to consumers in the form of higher wages. Existing JCT/CBO scores on surprise billing fixes’ premium effects suggest wages could increase by tens of billions of dollars if legislation is enacted.
Further, certain providers whom patients do not choose and cannot reasonably avoid, such as anesthesiologists and emergency room physicians, charge exorbitant out-of-network rates and use the threat of surprise billing as negotiation leverage with insurers, allowing them to extract excessively high in-network rates as well. These physicians often have median in-network rates that exceed 4 to 5 times what Medicare pays for the same service, compared to much lower rates for other physicians.
In many cases, these same providers are backed by private-equity funded groups who purposefully exploit this market failure as part of their business model, profiting from surprise billing at the expense of families. These private equity firms reap so much in profits from surprise billing that they have engaged in an aggressive $53 million lobbying and ad campaign to stop Congressional action or to secure a solution that allows them to maintain — or even increase — their revenue.
Myth 2: Using a locally-based market rate to end surprise billing would massively disrupt the health care system, resulting in clinician shortages and potentially even hospital closures.
Reality: Even the proposals with the largest spending reductions affect only a small share of overall provider revenues and the subset of physicians who routinely engage in surprise billing — making massive systemic disruption unlikely. These physicians currently receive inflated payments because of surprise billing and would be paid reasonable, market-based rates under the proposal.
Surprise bills are only a small fraction of business for most hospitals and providers — raising questions about why opponents to a surprise billing fix say a local market-based rate will “shred the [U.S. health care system] safety net.” Current Congressional proposals do not cut funding to any federal health care programs such as Medicare, Medicaid, and the Children’s Health Insurance Program. In addition, a 2019 piece estimated that the impact on physician and hospital revenues is expected to be marginal — only 0.75 percent to 1 percent between 2020 and 2029 — while aggregate hospital and physician revenues are expected to rise by more than 60 percent, or $1.6 trillion during the same time frame.
Those who are most likely to see an impact are a small subset of provider types that use surprise billing — and the threat of surprise billing — as a tactic to reap higher payments. Many surprise bills are thousands of dollars, with some greater than 600 percent more than Medicare would have paid for the same service. A recent Health Affairs study found that, on average, anesthesiologists are charging up to 802 percent of Medicare rates for out-of-network services — while already making 367 percent of Medicare rates for the same services in-network. These specialty physicians who routinely provide out-of-network care are also highly compensated; for example, in 2017, emergency medicine physicians were paid an average salary, after expenses, of $352,697, while radiologists were paid an average of $488,338.
The surprise billing phenomenon is unrelated to access or shortage issues. Allowing it to continue is not an adequate or rational solution for solving these issues, and in fact further harms patients.
Myth 3: The benchmark approach uses “government rate-setting” to fix surprise billing.
Reality: Current solutions to fix surprise billing rely on market rates set through negotiations between providers and insurers to determine the payment for out-of-network services.
Surprise billing has arisen from a clear market failure. Many providers are highly consolidated, giving them significant market power. Some — often backed by private equity — are able to gain additional leverage by remaining out-of-network and “balance billing” patients. The proposed solution of a locally-based market rate would reflect local market forces and in-network rates. Establishing a payment standard for out-of-network services does not change providers’ existing market power, which they can continue to exercise to negotiate their in-network rates.
A locally-based market rate also adds a level of certainty and predictability in regards to payment for out-of-network care for insurers (who will build uncertainty into rates), providers, and American families.
The alternative solution pushed by some providers — arbitration — adds more complexity and uncertainty to the health care system, as well as more government bureaucracy. Hospital and emergency care often results in a surprise bill; in 2016, more than 40 percent of emergency department visits and inpatient admissions at in-network facilities resulted in a surprise bill. Determining payments for these bills through arbitration establishes a new bureaucratic process, resulting in increased administrative costs that will be paid by consumers, employers, and taxpayers. Furthermore, the New York state experience is informative: Arbitration decisions average 8 percent higher than the 80th percentile of charges, resulting in upward pressure on commercial rates and premiums.