The Wall Street Journal reported this week that Arnold Ventures is using another tactic in its long-running battle against hospital consolidation, a huge driver of high and rising health care prices: litigation. AV is helping to fund Fairmark Partners — a group pursuing antitrust lawsuits against hospital behemoths in Wisconsin, Connecticut, and North Carolina. (AV will not benefit financially from these cases). The suits allege these systems use their market power to crush competitors and illegally inflate health care prices, the WSJ reported. Excessive health care prices in turn lead to high and rising health care costs for consumers, employers, and taxpayers.
“Hospital systems too often use their market power to engage in anticompetitive behavior, which acts as a tax on patients, companies and taxpayers,” AV Co-Founder and Co-Chair John Arnold tweeted in response to the piece. “With government slow to respond [and] without the resources to investigate, Arnold Ventures helps fight to reduce costs.”
Big hospital systems are aggressively acquiring smaller hospitals and physician practices, consolidating the market and crushing the competition. Today, about 90% of metropolitan hospital markets in the U.S. are highly concentrated, and more than one in three physicians now works directly for a hospital or a practice at least partially owned by a hospital. Many regions are dominated by a single system. These dominant systems then charge more, threatening access because patients are afraid of unaffordable bills or forcing families into debt outright when they seek necessary care.
Number of physicians now working directly for a hospital or a practice at least partially owned by a hospital
Consumers and employers are already deeply engaged in the fight against the monopolistic business practices of health systems. In 2019, Sutter Health agreed to a landmark settlement of $575 million to resolve charges that it engaged in anticompetitive business practices against consumers and employers — a first-of-its-kind legal case against the hospital industry. In that case, employers led the effort, which was later joined by then-California Attorney General (now HHS Secretary) Xavier Becerra.
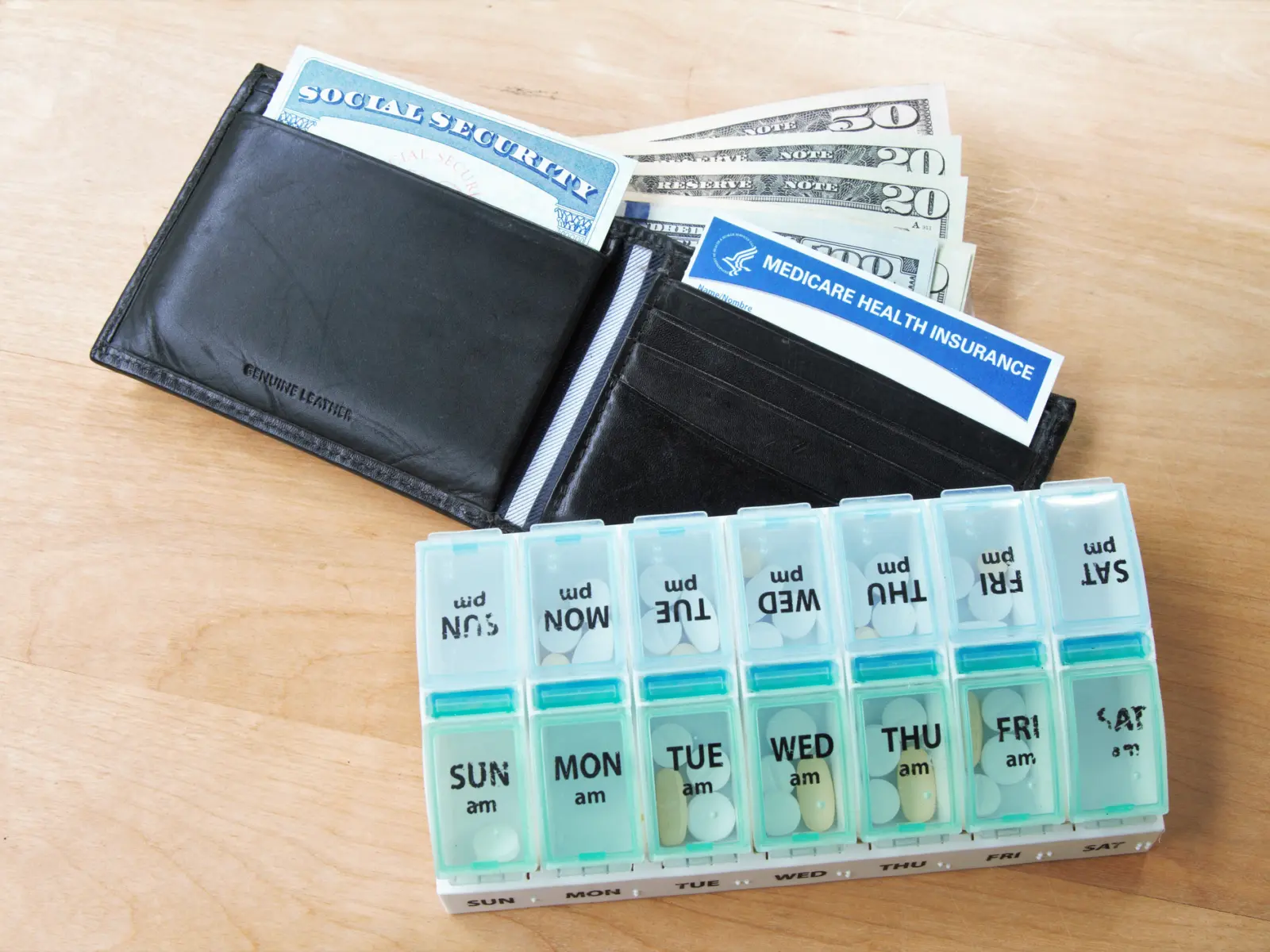
Families, patients, and employers bear the brunt of hospital consolidation.
“This is fundamentally about employers and others in the environment responding to the very real problem of high and rising prices,” said Erica Socker, vice president of health care for Arnold Ventures.
Lawsuits are just one tool stakeholders and policymakers are using to address health care prices and to lower health care costs, and momentum continues to build. Federal policymakers are increasingly indicating their interest in taking on hospital consolidation — with the Federal Trade Commission and U.S Department of Justice hosting a series of listening sessions this spring on the firsthand effects of mergers and acquisitions and members of Congress pursuing hearings on the issue.
State policymakers and regulators are also taking action. Some states are using existing authorities to take on behemoth systems. In Massachusetts, an independent state agency there made a first-of-its-kind move to hold a dominant health system accountable for its role in driving state health care spending higher. Oregon passed legislation to strengthen its merger review authority in 2021, and California’s Assembly recently passed legislation banning anticompetitive contracting practices that large hospital systems use to limit competition from lower-priced competitors — bringing it one step closer to enacting these protections.
In Indiana, lawmakers continue to call for lower prices and passed hospital price transparency legislation in 2020. In North Carolina, the attorney general is hosting a series of public listening sessions on consolidation’s impact on patients and local communities, while the state’s treasurer has taken a number of steps to shed light on high hospital prices and help advance policy solutions to increase price transparency, improve community benefit, and reduce medical debt.
Across all of AV’s work to fix the broken hospital market, data is in the driver’s seat. AV has funded a range of research efforts to understand the drivers and consequences of high prices and consolidation and to inform effective policy solutions, as well as new tools to bring data about hospital prices and finances to light.
The Employers’ Forum of Indiana, an AV grantee, launched a new hospital price transparency resource called Sage Transparency in May 2022. This interactive, freely accessible dashboard allows employers, researchers, and policymakers to compare hospital price and quality for more than 4,000 hospitals, incorporating data from the RAND Hospital Price Transparency Study, Turquoise Health, AV grantee National Academy of State Health Policy’s Hospital Cost Tool, and the Centers for Medicare & Medicaid Services, among other sources.
Writ large, abusive practices — including by hospitals — that increase prices and health care costs abound in our health care system and are at the forefront of AV’s work.
“Health care ultimately needs to be affordable to those who pay for it: taxpayers, employers, and households,” said Mark E. Miller, executive vice president of health care for Arnold Ventures.